TRAUMATIC PATELLAR DISLOCATION
Patellar dislocation occur as a result of a twisting injury with strong contraction of the quadriceps.
An acute effusion may develop, and this diagnosis may be mistaken for the more common anterior cruciate ligament injury. The patella usually reduced easily with extension of the knee, and the patient may never have appreciated that the patella was dislocated.
Acute injury often are accompanied by a large effusion and knee tenderness. Occasionally the patella may be so unstable that simple range of motion may displace it.
X-Ray of the right knee. The normal position of the patella in the knee joint
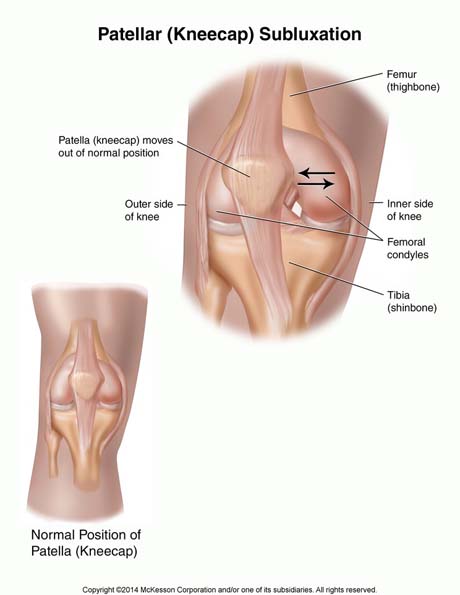
Up: Patellar lateral dislocation
Down: Normal patellar position.
The injured left knee is swollen due to patellar dislocation.
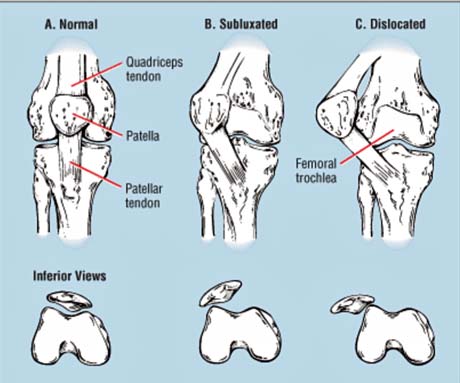
The medial structures is ruptured after acute patellar dislocation.

The patella is dislocated laterally. The medial patelofemoral ligament was torn.

Right knee MRI. Lateral patellar dislocation due to trauma


3D reconstruction of the right knee. Traumatic patellar dislocation
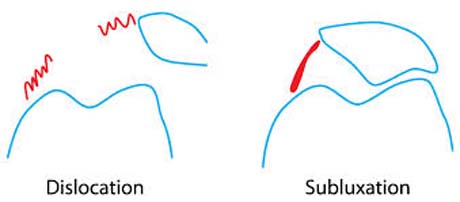
Medial patellofemoral ligament torn due to traumatic patella dislocation (red arrow)


